An impulsive relationship or purchase may seem like a stroke of genius, but it can also be a symptom of a manic phase.
In recent years, the term “bipolar” has slipped into everyday conversation, often misused to describe simple mood swings. However, tossing the term around lightly trivializes a serious, complex, and potentially debilitating mental health condition when left untreated. Psychiatrist and addiction specialist Xavier Fábregas offers clarity on what bipolar disorder really entails—a condition far more impactful than many realize.
Bipolar disorder is defined by alternating depressive episodes and manic or hypomanic phases. This swing between emotional extremes complicates diagnosis. While depressive episodes may resemble standard depression, manic phases often go undetected: the person feels energetic, productive, and even euphoric—making them less likely to seek help.
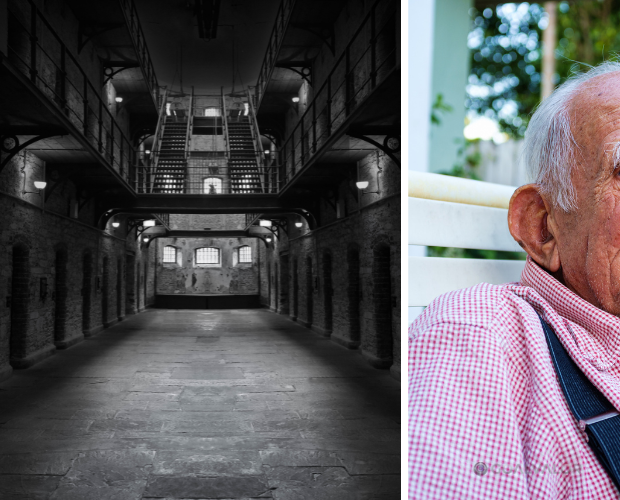
Fábregas emphasizes that true bipolar disorder has little to do with mood fluctuations caused by external events. Manic phases manifest through reduced sleep needs, hyperactivity, impulsive decisions, and a distorted sense of reality. These episodes can last for weeks and seriously impact personal and professional life. One patient, for example, impulsively bought a house—completely unaware they were in an altered state of mind.
This is where the disorder stops being internal and begins to have real-world consequences. Making high-stakes decisions—financial, relational, or otherwise—without realizing one’s mental state is compromised should be a red flag. Bipolar disorder can easily hide behind a façade of high energy and productivity, which is exactly what makes it dangerous.
Treatment usually involves mood stabilizers, antidepressants, and antipsychotics depending on the phase. The goal is not merely to “cheer up” or “calm down,” but to stabilize the emotional cycle and prevent relapses. Mismanaging medication can cause what's known as a “phase switch”—where the patient spirals from depression into a dangerous high due to inappropriate treatment.
. Bipolar disorder can easily hide behind a façade of high energy and productivity, which is exactly what makes it dangerous.
A proper diagnosis must consider not only symptoms but also the person’s family, social, and work environment. These contexts are vital for detecting imbalances early and offering support. In the workplace, where decisions are constant and often high-stakes, colleagues and supervisors should be aware and educated—ready to intervene or accommodate when necessary.
Perhaps the biggest danger is stigma. Using “bipolar” as an insult or casual descriptor fuels misinformation and social rejection. “It’s as simplistic as saying ‘I’m depressed’ without understanding clinical depression,” Fábregas warns. These throwaway comments reinforce myths and diminish the reality of a serious—and sometimes fatal—condition.
Emerging from a manic or depressive phase isn’t quick or easy. It often requires hospitalization, close supervision, and major lifestyle adjustments. Fábregas stresses that patients aren’t acting this way by choice, but due to a deeply altered perception of reality. “It’s not about delusions like believing you’re Napoleon,” he explains, “but about a sense of omnipotence that can spiral into complete loss of control.”
The takeaway is clear: we must stop using clinical terms as slang and begin speaking about mental health with the respect, accuracy, and seriousness it deserves. Because a diagnosis isn’t an adjective—and people’s lives depend on us understanding that in time.
#RealBipolarity #EmotionalEducation #StopStigma #ImpulsiveDecisions